Pelvic Organ Prolapse – An Overview
Feeling of heaviness in vaginal area? pressure in your pelvis?
Do you experience an annoying feeling of “heaviness or bulge” in the vaginal area or a “pressure” between the vagina and anus or pelvis?
It is usually a part of a range of clinical conditions caused by Pelvic Floor Dysfunction, vaginal bulging, and a symptom of Pelvic Organ Prolapse.
This can be a very distressing condition for women. If you suffer from Pelvic Organ Prolapse, you may feel embarrassed if others know of your condition, as it is not something that anyone talks about openly. There may be a fear of talking to your family doctor or gynecologist about the condition, and there are chances of it being misdiagnosed by the medical profession.
What is pelvic organ prolapse?
Pelvic organ prolapse is a condition in which one or more of the pelvic organs (uterus, bladder, rectum, or vagina) drops down from its normal position and presses against the wall of the vagina, causing protrusion of organs into the vagina. In some cases, the prolapsed organ may protrude through the vaginal opening. Pelvic organ prolapse is most common in women who have had one or more vaginal births.
Pelvic Organ prolapse is related to symptoms from a failure of the supporting structures, the pelvic floor muscles, resulting in collapse, causing protrusion of organs into the vagina.
There may be a descent of the bladder into the anterior vaginal wall, the rectum into the posterior vaginal wall and the vaginal vault or uterus into the apex of the vagina.
How common is pelvic organ prolapse?
A recent study reported that pelvic organ prolapse is a common condition affecting nearly 30% of women (20–59 years of age) and more than 50% over 50 years of age seeking gynecologic clinic visits. Women with Pelvic organ prolapse often present with a combination of pelvic floor disorders, such as incontinence, bowel, bladder, and sexual dysfunction (Sánchez-Sánchez et al., 2020).
Pelvic organ prolapse symptoms:
Symptoms commonly are reported as:
- A feeling of pressure or heaviness in the vaginal area
- Presence of a bulge in the vaginal space and at the entrance of the vagina
- Stress urinary incontinence – leaking urine with coughing, sneezing, jumping, sit to stand etc.
- Constipation
- Difficulty emptying bladder
- Symptoms worsen through the day of activity
- Symptoms improve with rest and lying down
Factors contributing to pelvic organ prolapse
- Weakness in Pelvic floor muscles and laxity in connective tissue supporting the organs. It can occur during pregnancy and childbirth, having multiple vaginal births, birth trauma from forceps and can influence pelvic organ prolapse.
- Increase in intra-abdominal pressure above from chronic coughing, chronic constipation, high-level stress with abdominal tension, and heavy lifting, causing pressure going down to the organs below.
Risks for pelvic organ prolapse

- Older age
- High parity / multiple pregnancies
- Obesity
- Early age at the first delivery
- Forceps delivery
- A prolonged second stage of labour
- Carrying and lifting heavy objects or doing heavy work
- High infant birth weight
Types of prolapse :
Uterine prolapse – Uterus descending and dropping down into the vaginal space
Vault prolapse – Can Occur after a hysterectomy, where the top portion of the vagina sinks into the vaginal space
Cystocele – Bladder pushing on the front of the vagina
Rectocele: the rectum bulging from the back of the vaginal wall. A clinical study noted that most women presenting with prolapse complained of obstructed defecation and clinically were noted to have had posterior-compartment prolapse (Dietz et al., 2018)
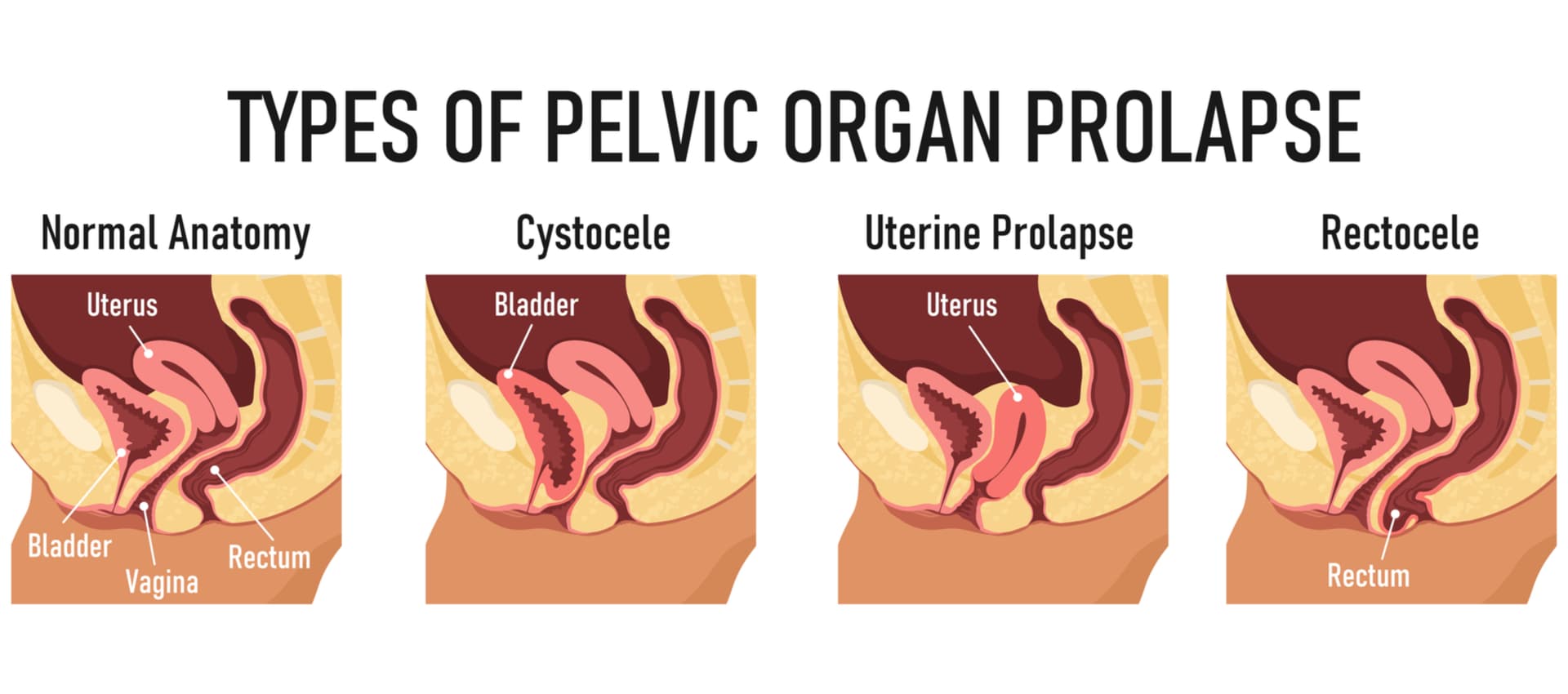
*It is not uncommon to have more than one prolapse occurring at the same time*
Sexual dysfunction with Pelvic Organ prolapse is prevalent in women, frequently reporting having less sexual desire, arousal, orgasm, and pain, with negative implications on their relationship with their partners ( Lucia La rosa et al., .2019)
Most women do not mention these issues unless specifically asked about them. Although pelvic organ prolapse does not pose any risks, however, women with this problem are known to report a lot of distress, decreased quality of life with reduced physical activity and limitations in social, sexual, and occupational performance.
Management and treatment for prolapse:
Surgery for prolapse:
Surgery usually is opted for patients with severe prolapse, at least stage II prolapse or bothersome symptoms and have failed the conservative approach.
It is done to relieve the symptoms, restore normal anatomy, prevent relapses and correct possible intrapelvic defects.
A surgical approach can vary depending on the condition.
- Sacral colpopexy ( for uterine prolapse) and sacrospinous ligament fixation ( for Vault prolapse repair)
- Anterior colporrhaphy ( Cystocele repair )
- Posterior colporrhaphy ( Rectocele repair )
- Perineorrhaphy ( repairs to the perineal body to help relieve the symptoms of vaginal bulge or laxity) to maintain bowel and sexual function.
- Obliterative procedures – are more appropriate and are usually considered in older women with advanced-stage prolapse, who cannot tolerate extensive surgery and no longer desire preservation of coital function.
According to some studies, surgical management of POP improves the long-term quality of life and sexual response. However, conversely, other studies describe the worsening of sexual function in patients and dyspareunia (pain during sexual intercourse or sexual activity ) following surgical treatments. Also, studies have noted complications and risks following surgery, including mesh erosion into the vagina, infection, bowel dysfunction, stress incontinence, revision surgery etc.
Faced with this evidence, the authors noted that a multidisciplinary approach to the treatment of women with POP and cystocele is essential (Lucia La rosa et al., .2019)
Conservative pelvic organ prolapse treatment and management:
Research indicates that Conservative-based approaches and interventions help women regain control over the prolapse symptoms and their life. There is an increased need for providing education among women and health care professionals on preventative measures and available conservative multi-professional team-based approaches. With treatment options expanding to include conservative choices, women presenting with this condition or symptoms need to be listened to, given better information about available treatment choices and offered support in making an appropriate decision that is right for them (Abhyankar et al. 2019)
*It is vital to create more awareness of pelvic organ prolapse and its symptoms among women in making appropriate treatment choices that are right for them.*
Pessaries :
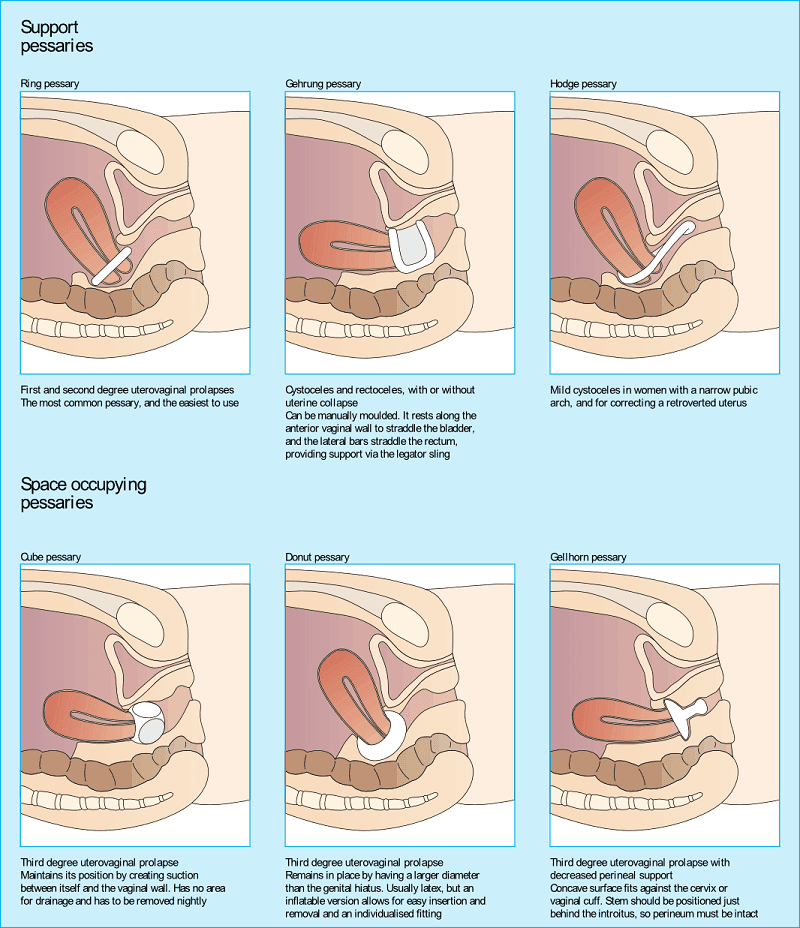
Vaginal pessaries are intravaginal support devices used to reduce prolapse or incontinence. They are medical-based silicone devices inserted into the vagina to help hold the organs up in place. They are alternative non-invasive treatment options and are usually controlled by the patient. It is known to provide symptom relief without surgical complications for women with these conditions. Pessary use is also known to be the most cost-effective treatment alternative for treating pelvic organ prolapse (Radnia et al., 2019)
Some women, although were successfully fitted with a pessary for prolapse, one-third were noted to undergo surgery, with approximately 60% of women undergoing surgery within the first year and 90% within two years. ( Patnam et al., 2020)

Pelvic floor physiotherapy for pelvic organ prolapse:
PFM training and Pessaries can be valuable therapeutic tools to relieve symptoms of POP and for a conservative approach.
Physiotherapists trained in Pelvic Floor Physiotherapy can help assess tissue laxity and muscle strength and provide appropriate management options from pelvic floor muscle training and relaxation training to address the pressure system from above or below as part of prolapse physio treatment. Pessaries management or provide appropriate referrals to address the dysfunction.
Physiotherapy-based treatment for Pelvic Organ Prolapse is identified in research and has focused on prevention, early diagnosis, and treatments.
Pelvic floor physiotherapy exercises prescription and monitoring are useful in treating and preventing functional disorders of the pelvic floor. Proper prolapse physio or physiotherapy for pelvic organ prolapse is essential for individuals experiencing pelvic organ prolapse to manage their symptoms effectively.
Patients with pelvic organ prolapse symptoms should seek the expertise of a prolapse physiotherapist to address their pelvic floor dysfunction.
In Conclusion, education and awareness are vital among women and professionals in taking conservative approaches for pelvic organ prolapse as a first line of management and preventative measure, with a multi-professional team approach in treatment decision-making.

Cynthia Pathipati – Registered Physiotherapist
Cynthia Pathipati completed her bachelor’s in physiotherapy and is a qualified Registered Physiotherapist in good standing with the College of Physiotherapists of BC with more than 15 yrs of experience. She has Post-Graduate Credentials and Certifications as well as extensive knowledge experience in treating pelvic floor, orthopedic, neurological, vestibular and pain conditions.