Physiotherapy For Pelvic Pain – What You Need to Know
Pelvic pain is a common condition yet a complex problem that can affect both men and women. Pelvic pain is a pain or discomfort present between your lower abdomen from the belly button to the groin area. They could be symptoms of pain arising from the reproductive, urinary, digestive, and musculoskeletal systems.
Pelvic pain is part of Pelvic Floor Dysfunction, which is usually caused by tight pelvic floor muscles. If the muscles are tight, it can cause pelvic pain, urinary/fecal urgency and frequency issues.
Find more about pelvic floor dysfunction physiotherapy treatment.
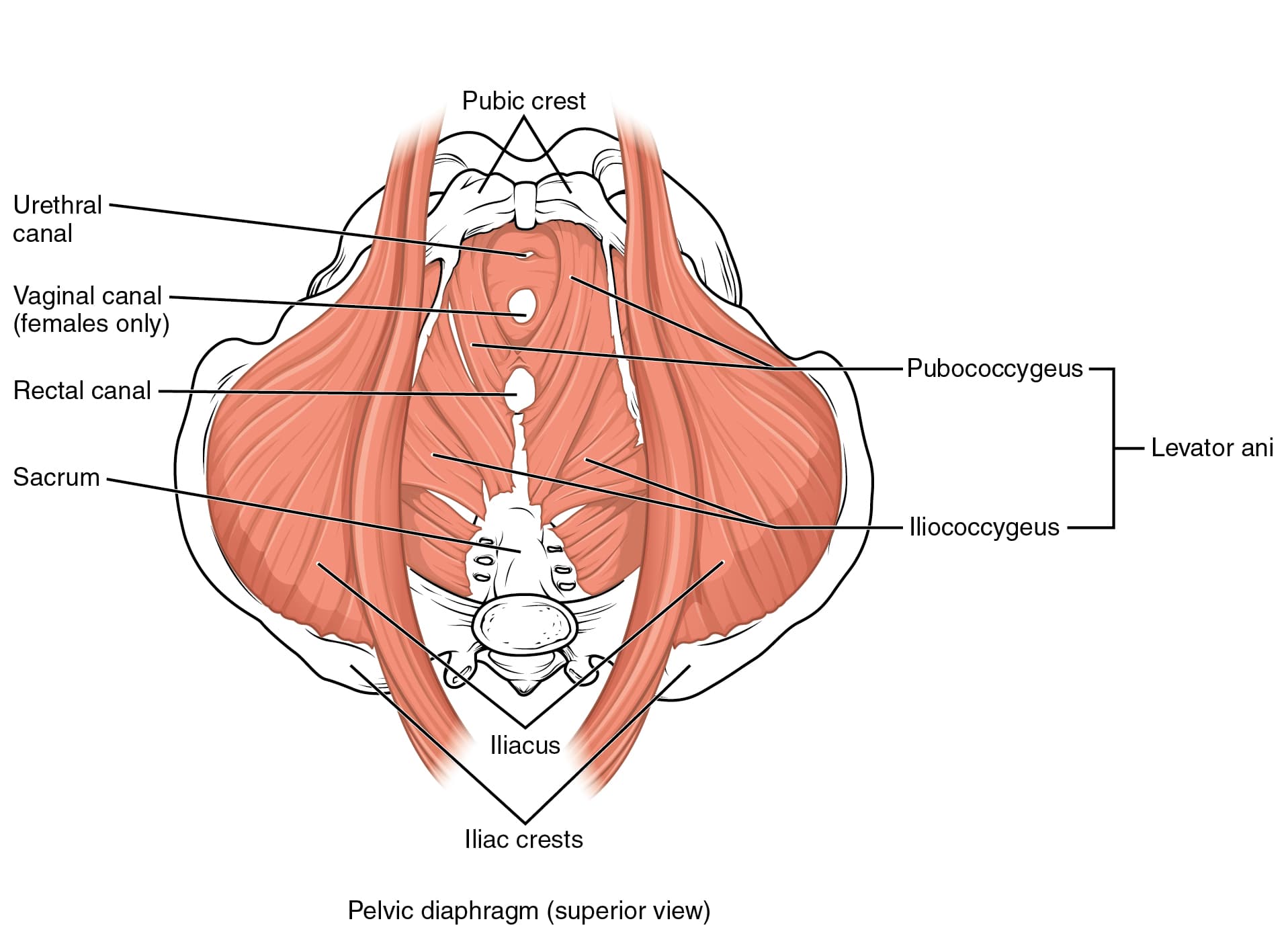
Learning about the layers of the pelvic floor, Pelvic floor muscles and fascial connections that envelope the deep pelvic area helps us understand more about pelvic pain.
Layers of Pelvic Floor and Perineum: there are known to be three layers which include
Layer 1: Superficial perineal muscle layer – urogenital triangle – It stabilizes the perineal body, supports the pelvic floor and propels semen expulsion, influences penile rigidity in males and voluntary sphincteric action of the anal canal in both men and women
Layer 2: Deep perineal muscle layer of the Urogenital Diaphragm – is essential for maintaining a continence mechanism.
Layer 3: Pelvic Diaphragm – includes Levator ani (PFM), coccygeus, piriformis, and obturator internus muscles. These support the internal pelvic organs, provide voluntary control of sphincteric action of the anal canal, and help and support the tailbone and hip lateral rotation movement.
Pelvic floor muscles (PFM), also known as Levator Ani muscles, support and protect the connective tissues that lay in your pelvic region from excessive load. The connective tissues include bone, tendons, ligaments, cartilage, and fat tissues. The PFM can be exercised to strengthen if weak or to lengthen if it is tight.
Fascial connections of the pelvic floor:
Fascia is the lining of the internal organs and muscles made of smooth muscle fibres, ligaments, blood vessels and connective tissue. Fascia covers and supports the inner organs like the bladder, intestines and uterus. Some of the ligaments connect to the lumbar spine and pubic symphysis. This fascial layer cannot be exercised.
The pelvic diaphragm and the urogenital triangle are all supplied by the Pudendal nerve. The only nerve that has both sensory, motor fibers and autonomic fibers is the Pudendal nerve. The sensory fibers of the pudendal nerve can lead to perineal and pelvic pain.
5 Important pelvic floor muscle functions:
Pelvic floor muscles provide various functions that help maintain pelvic integrity and harmony.
- Support: PFM provides internal pelvic organs like the uterus, bladder, and rectum support against gravity and intra-abdominal pressure
- Sphincteric: pelvic floor functions to control the continence mechanisms coordinating between the bladder, urethra (pee hole) and muscles
- Sexual: pelvic floor muscles help react to sexual stimuli by providing tone in vaginal and rectal canals and increased blood circulation to sexual organs and involuntary contractions during orgasm in both men and women.
- Stability: provides stability to the SI joint, pubic Symphysis, pelvic, lumbar, and hip joints, and functions to unload the spine (Hodges 2007).
- Sump- Pump: helping with venous and lymphatic circulation.
Acute and Chronic Pelvic Pain:
Acute pelvic pain:
Acute pelvic pain is the lower abdominal or pelvic pain of sudden acute onset, lasting less than three months. It is challenging to evaluate due to broad differential diagnosis and has different signs and symptoms that can be non-specific.
- Idiopathic pelvic pain
- Pelvic inflammatory disease
- Acute appendicitis
- Ovarian cysts,
- Ectopic pregnancy
- Endometriosis
- Cancer among postmenopausal women
These require medical attention and intervention ( Amit et al., 2016 ).
Chronic pelvic pain:
Chronic pelvic pain is pain and inflammation in the pelvic organs for more than six months. Chronic pain represents a syndrome that combines dysfunction of the pelvic floor muscles with the malfunction of pain perception linked with psychological and cognitive factors. ( Grinberg et al. 2020) A physiotherapist can help with these conditions.

- Vulvodynia
- Vestibulodynia
- Dyspareunia
- Vaginismus
- Chronic urological pain syndromes – include interstitial cystitis and Bladder pain syndrome.
- Dysmenorrhea
- Pelvic congestion Syndrome
- Coccydynia
- Anal fissures
- Chronic prostatitis
- Pudendal Neuralgia
Chronic pelvic pain: Most common causes
- Tight pelvic floor muscles or fascial tension
- Connective tissue dysfunction
- Neural tension along the nerve pathway
- Increase tension in the internal organs of the lower abdomen, including the bladder, prostate, uterus and ovaries.
- Pelvic congestion from varicose veins and poor circulation in the pelvic floor muscles
- SI joint /Sacroiliac joint dysfunction
- Genitourinary syndrome of Menopause due to hormonal changes
- Upregulation of the sympathetic nervous system from chronic stress, anxiety, catastrophization or depression leads to Persistent pain in the absence of actual tissue dysfunction or persistent pain states with a blend of tissue dysfunction.
What does the research say about physiotherapy treatment for pelvic pain:
Pelvic floor physiotherapy is useful in training the pelvic floor muscles, increasing the support of the bladder and uterus, and decreasing the strain on fascial connections, which can help improve your pain.

Releasing the pelvic floor and the fascia layers through pelvic support physiotherapy can help with non-mechanical back pain that can be caused by tight pelvic floor muscles, and the therapeutic interventions in chronic pain should follow a multidisciplinary approach( Grinberg et al. 2020)
Recent quality studies noted significant clinical effects of physiotherapy for chronic pelvic pain and female sexual dysfunction. The experts advocate a holistic and multidisciplinary approach that includes physiotherapy ( Bergman’s B 2018 )
Pelvic floor physiotherapists can help:
A physiotherapist specializing in pelvic floor problems can help you understand your problem and identify the appropriate solution.
Physiotherapy treatment for pelvic pain involves a biopsychosocial approach to your problems that begins with effective interviewing to understand your problem/ condition. Physical and biomechanical evaluation includes external and internal myofascial assessment, providing neurophysiology-based pain education to the condition. Therapeutic interventions can range from exercises, relaxation training, movement practice, myofascial release and connective tissue mobilization. Self-care/self-management and lifestyle modification approach to better assist with the treatment.
Physiotherapists at Opal Physiotherapy can help you in your journey toward recovery by setting realistic short and long-term goals that involve you being an active participant.
If you think you have pelvic pain and are diagnosed by your health care provider for having any of the pelvic pain conditions and need treatment for pelvic pain, do contact our clinic at 604-532-7887 or email [email protected] to get assessed and to start your recovery process.

Cynthia Pathipati – Registered Physiotherapist
Cynthia Pathipati completed her bachelor’s in physiotherapy and is a qualified Registered Physiotherapist in good standing with the College of Physiotherapists of BC with more than 15 yrs of experience. She has Post-Graduate Credentials and Certifications as well as extensive knowledge experience in treating pelvic floor, orthopedic, neurological, vestibular and pain conditions.