Guide To Pelvic Floor Dysfunction
Many people suffer from pelvic floor dysfunction for years. Unfortunately, there is very little understanding of this problem and the available pelvic floor dysfunction treatment options.
In most cases, many people who experience pelvic floor dysfunction avoid the conversation because it raises feelings of embarrassment. However, it is well-known that research and studies do not usually reflect the full extent of the issues.
Examining the prevalence of individuals silently enduring pelvic floor dysfunction challenges is noteworthy. More people go through the discomfort and pain associated with these issues without seeking help or support. It can be a lonely and daunting experience before recognizing the symptoms and seeking pertinent information.
However, with the power of modern technology at our fingertips, those experiencing pelvic floor problems can easily search for information online or connect with others who have gone through similar experiences.
Sometimes, it takes a chat with a trusted physician or physiotherapist to relieve the situation. We must break the silence surrounding pelvic floor issues and encourage individuals to seek the help and support they need.

Did you know that pelvic floor dysfunction can affect people of all ages?
A study by the American Academy of Family Physicians found that dyspareunia, a type of pelvic floor dysfunction, is a common condition and can affect women’s mental and physical health. Furthermore, according to Pelvic Health Solutions, 3 million Canadians suffer from incontinence, with 1 in 3 women, 1 in 9 men, and 1 in 6 children under 17 years being affected.
Pelvic floor dysfunction impacts physical function and can interrupt sexual function, health and psychological well-being. That’s why anyone who suspects they may be suffering from this condition should visit their healthcare provider for an accurate diagnosis and treatment.
Research in Canada suggests pelvic floor dysfunction can affect people of all ages. According to a study by a professor at the University of Montreal, 90% of cases of incontinence in women can be improved with exercise, and 70% of cases can be treated with physiotherapy.

A pelvic floor physiotherapist can help!!!
It is essential to seek professional help to address pelvic floor dysfunction. A pelvic floor physiotherapist is a highly trained health professional who can help diagnose and treat pelvic floor dysfunction using exercise, education, and behavioural modification techniques.
They can also provide personalized treatment plans and support to help individuals manage their symptoms and improve their pelvic health. Seeking the help of a pelvic floor physiotherapist is crucial, especially when traditional treatments such as medication and surgery have proven ineffective.
Working with a pelvic floor physiotherapist helps individuals regain control of their bladder and bowel, reduce pain and discomfort, and improve their quality of life.
It is vital to spread awareness to help people with pelvic conditions get diagnosed earlier and to be able to see a pelvic floor physiotherapist to address their pelvic floor disorder.
What is a pelvic floor?
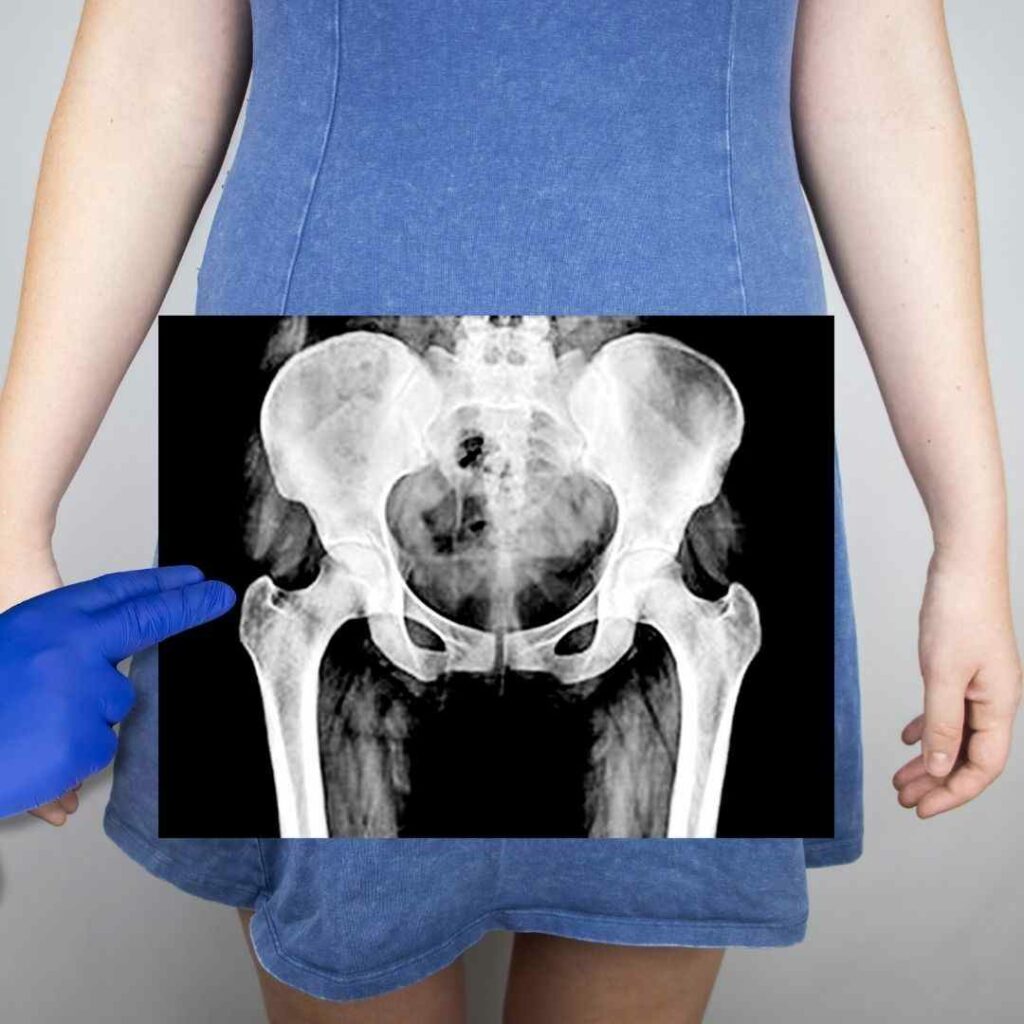
The pelvic floor consists of several muscles, ligaments and tissues which support the bladder, rectum and sexual organs in men and women by wrapping them around the pelvic bone.
The contraction and relaxation of this pelvic muscle system help with managing the bowels and bladder function. Therefore, it is only through the appropriate muscle performance that urination, defecation, and intercourse for women and men are allowed.
When this supportive system does not function well, a common health issue appears called pelvic floor dysfunction (PFD), causing several distressing symptoms.
What is pelvic floor dysfunction (PFD)?
Pelvic floor dysfunction is a term used to describe a range of problems that can occur when the pelvic floor muscles, ligaments, and connective tissues are weakened, tight, or have difficulty coordinating.
Pelvic floor dysfunction can manifest differently depending on the underlying issue.
Types of pelvic floor dysfunction
Several types of pelvic floor dysfunction can affect both men and women. Some of the most common types of pelvic floor dysfunction include:
Bladder dysfunction: Urinary incontinence is when a person has difficulty controlling their urine flow, leading to involuntary leakage of urine and an overactive bladder.
Bowel dysfunction: Fecal incontinence is when a person has difficulty controlling their bowel movements, leading to the involuntary leakage of stool.
Sexual dysfunction: This can include
- Pain during sexual intercourse
- Difficulty achieving orgasm
- Decreased sexual desire
- Erectile dysfunction
Pelvic organ prolapse: Descent of a woman’s internal organs, such as the bladder, uterus, or rectum, from the normal anatomical position into the vaginal canal or outside. It can include uterine prolapse, Cystocele, Rectocele / rectal prolapse, Enterocele and Urethrocele.
Pelvic pain: Pain or discomfort in the pelvic region, which various factors, including pelvic muscle tension, nerve damage, or inflammation, can cause.
Levator ani syndrome: It is a condition distinguished by chronic pelvic pain caused by tension in the pelvic floor muscles.
Chronic constipation: This is a condition in which bowel movements are infrequent, difficult, or incomplete.
Interstitial cystitis: Pelvic floor dysfunction has been reported to exacerbate interstitial cystitis (IC) symptomatology and has been associated with events such as bladder inflammation, postural instability, sacroiliac malalignment, and trauma. It is believed that PFD can contribute to bladder dysfunction by causing urinary urgency, frequency, and pain. Patients with IC should be evaluated for PFD, and treatment for both conditions may involve pelvic floor physical therapy.
Proctalgia Fugax: Proctalgia fugax is a type of rectal pain caused by muscle spasms in the pelvic floor muscles. PFD has been identified as a possible cause of proctalgia fugax, as the pelvic floor muscles regulate bowel movements. In some cases, PFD can cause the muscles to become too tight or too weak, leading to difficulty with bowel movements and increased pain and discomfort in the rectum.

Causes of pelvic floor dysfunction
Physicians and other associated health care professionals relate PFD with risk factors and cause that weaken the areas of muscles or injure the connective tissue, such as :
Pelvic floor dysfunction symptoms
Pelvic Floor Dysfunction can be an uncomfortable and challenging condition to live with. The symptoms vary among individuals, and it can also depend on the severity of the condition. Some common symptoms can include

Who is affected more by PFD?
Pelvic floor disorders (PFD) affect certain populations more than others:
- Women are more affected by PFD than men. One in three women suffers from PFD, while men typically experience PFD post-prostatectomy or following radiation.
- PFD prevalence increases with age in women. Nearly one-quarter of all women and more than one-third of older women report symptoms of at least 1 PFD.
- Obesity and higher BMI are associated with higher odds of one or more pelvic floor disorders in women. The prevalence of PFD increases with BMI, except in the case of pelvic organ prolapse.
- Vaginal childbirth is a strong risk factor for PFD in women under 60. Higher parity is associated with increased odds of PFD.
- PFD is less common in Asian women compared to other races/ethnicities.
- Socioeconomic factors play a role, with PFD being more common in women of lower socioeconomic status. Families of children with PFD had significantly lower socioeconomic status compared to controls.
A review of the impact of pelvic floor disorders on sexual function in women found that these conditions are common and often associated with a significant reduction in women’s psychological, social, and sexual well-being.
On the other hand, the prevalence in men appears to be dramatically lower. However, men tend to associate pelvic floor dysfunction more with prostatitis, post-prostate surgery, erectile dysfunction and premature or painful ejaculation, which often coexist with pelvic floor disorders.

How is the diagnosis made?
The diagnosis of pelvic floor dysfunction is made by reviewing the medical condition and history, evaluating patient symptoms, and doing a physical exam of the pelvic floor muscles for spasms, asymmetry in muscles, weakness, or misalignment in the hips/pelvis.
The most common medical examination can be external or internal and is a painless procedure which can involve:
How do pelvic floor physiotherapists diagnose pelvic floor dysfunction?
A physiotherapist can diagnose PFD by thoroughly assessing the pelvic floor and associated musculoskeletal system.
According to an article in the Journal of Women’s Health Physical Therapy, this assessment should include a detailed history, a musculoskeletal examination, and a pelvic floor examination, which may include an internal pelvic exam to assess muscle tone and strength.
During the pelvic floor exam, the physiotherapist will look for signs of hypertonicity or hypotonicity in the pelvic floor muscles, corresponding to increased or diminished activity. They may also assess for inappropriate coordination of the pelvic floor muscles.
The physiotherapist may use biofeedback, electrical stimulation and other techniques to assess muscle function and to help the patient learn to engage or relax the pelvic floor muscles as needed.
It is important to note that physiotherapists specializing in pelvic floor dysfunction may have different assessment protocols and treatment techniques. Larger, well-designed trials are needed to establish standard protocols.

Treatment for pelvic floor dysfunction with physiotherapy
Pelvic floor dysfunction treatment aims to reduce muscle tension and relax the muscle system for the patients to gain better control of their bowels and bladder. The most common techniques used in the realm of physiotherapy for PFD treatment that has been scientifically supported with evidence are:
Biofeedback
This is the more simple therapeutic method, performed with the assistance of a physical therapist. It is painless and considerably helpful. Electro pads are placed on the skin, or small probes are inserted into the anus or the vagina while the movement of the pelvic floor muscle function is monitored. Biofeedback is a method that the patients can also do on their own with appropriate equipment.
Pelvic floor muscle training (PFMT)
Pelvic floor muscle training is proven to be significantly effective for PFD treatment. In addition, research has shown that pelvic floor rehabilitation using pelvic floor muscle training gives greater results and offers progress in objective muscle strength, length, prolapse severity or subjective improvement in prolapse symptoms.
During pelvic floor muscle training, the patient learns pelvic floor contraction and relaxation of their pelvic floor muscles, activating the core and abdominal muscles appropriately. This can be done through a series of kegel exercises, such as squeezing and lifting the pelvic floor muscles, holding the contraction for a few seconds, and then releasing. Over time, the patient gradually increases the duration and intensity of the exercises.
To ensure the pelvic floor exercises are performed correctly, seeking guidance from a qualified healthcare professional, such as a physiotherapist specializing in pelvic floor health, is recommended. With regular practice, pelvic floor muscle training can improve pelvic floor function and quality of life.
Electrical muscle stimulation
The electrical current transferred (low-grade and therefore absolutely safe) to either the vagina or the anus through a small-sized probe stimulates the muscles to generate muscle contractions, which then helps to facilitate and strengthen the muscles of the pelvic floor area.
Ultrasound/low-level laser therapy (LLLT)
Therapeutic ultrasound and Low-Level Laser Therapy are beneficial for treating pelvic pain. It helps in decreasing muscle tension and enhancing blood circulation. It also helps with treating scar tissue after a C-section or Episiotomy.
Lifestyle modifications

Daily lifestyle factors and habits that focus on self-care can significantly assist the treatment process. For example, meditation combined with some breathing exercises, practicing yoga, having warm baths, or trying acupuncture for relaxation is some of the effective stress-relieving and relaxing methods for the body.
Furthermore, consuming more fibre and fluids or taking certain medications, such as laxatives, can help improve the condition.
Refraining from causing excess pressure during urination or defecation has proven helpful.
Conclusion:
Pelvic floor dysfunction is a common condition affecting men and women of all ages. Various factors, including menopause, pregnancy, childbirth, aging, abdominal or pelvic surgery, and certain medical conditions, can cause it.
Pelvic floor dysfunction can cause various symptoms, including urinary incontinence and fecal incontinence, pelvic organ prolapse, chronic pelvic pain, sexual dysfunction, and constipation. However, the good news is that a qualified physiotherapist can effectively treat pelvic floor dysfunction using a combination of pelvic floor muscle exercises, bladder and bowel training, pain management, and lifestyle modifications.
If you are experiencing symptoms of pelvic floor dysfunction, it’s important to seek help from a healthcare professional specializing in pelvic floor health. You can improve your pelvic floor function and regain your quality of life with the right treatment.
Need Help With pelvic floor dysfunction? Contact us to learn more about how our Pelvic floor physiotherapist can help.

Cynthia Pathipati – Registered Physiotherapist
Cynthia Pathipati completed her bachelor’s in physiotherapy and is a qualified Registered Physiotherapist in good standing with the College of Physiotherapists of BC with more than 15 yrs of experience. She has Post-Graduate Credentials and Certifications as well as extensive knowledge experience in treating pelvic floor, orthopedic, neurological, vestibular and pain conditions.